By Zeena Johar, President – ICTPH
According to the United States National Library of Medicine, the term “Managed Care” encompasses “Programs intended to reduce unnecessary health care costs through a variety of mechanisms, including: economic incentives for physicians and patients to select less costly forms of care; programs for reviewing the medical necessity of specific services; increased beneficiary cost sharing; controls on inpatient admissions and lengths of stay; the establishment of cost-sharing incentives for outpatient surgery; selective contracting with health care providers; and the intensive management of high-cost health care cases.” The programs may be provided in a variety of settings, such as Health Maintenance Organisations (HMO) and Preferred Provider Organisations (PPO) and Point-of-Service (POS) Plan.
A health maintenance organisation (HMO) is a managed care organisation (MCO) that provides a form of health care coverage through hospitals, doctors, and other providers through contractual agreement. In the HMO Staff Model physicians are direct employees or comprise of a closed-panel wherein contracted physicians may only see HMO patients. In the HMO Group Model, the HMO contracts a multi-specialty physician Group Practice. The Group Practice may be established by the HMO and only serve HMO members (Captive Group Model). Kaiser Permanente is an example of a Captive Group Model. An HMO may also contract with an existing, Independent Group Practice (Independent Group Model), allowing the practice to treat non-HMO patients. An Independent Practice Association (IPA) contact with an HMO, allows empanelled physicians to also treat non-HMO members. In the Network Model, an HMO contracts with any combination of groups, IPAs (Independent Practice Associations), and individual physicians.
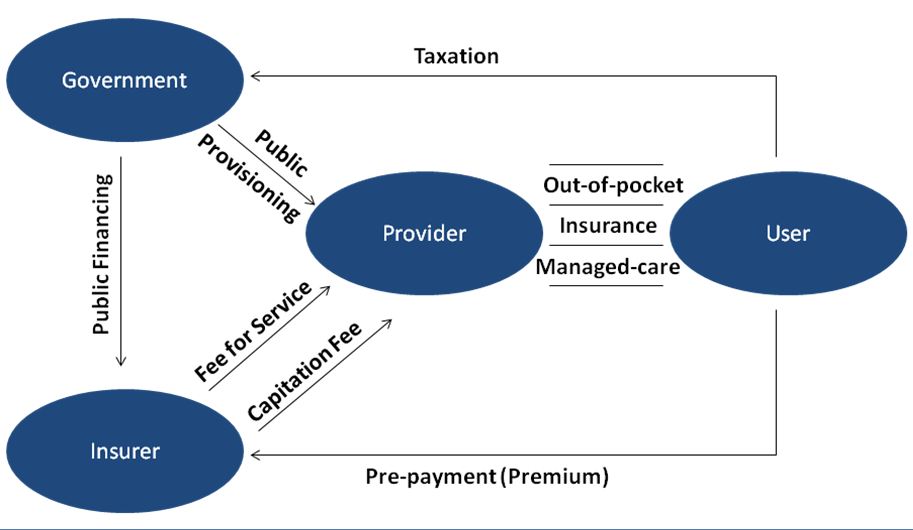
With 80% of healthcare expenditure being out-of-pocket (OOP) and only 0.9% accounted for as public expenditure presents us with an enormous opportunity to organize health care better so that it costs (the government or the individual) less but delivers more. Health insurance schemes in India targeting the vulnerable are on the rise but they are focused almost entirely on secondary and tertiary care to the total exclusion of primary care as well as any approaches towards dealing with underlying risk (and causal) factors. In our view there is a need for a disruptive approach to take us closer to the managed-healthcare delivery for our populations where protocol driven effective and accessible primary-healthcare, with established referrals to higher levels of care will organize the healthcare delivery market so that it is able to deliver health and well-being and not just curative care in a very narrowly defined context of secondary and tertiary care.
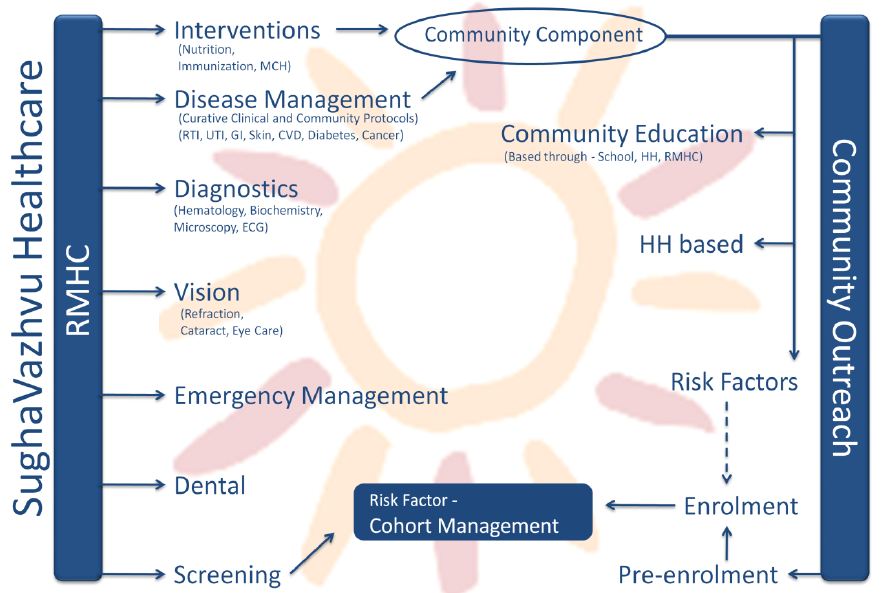
The first ICTPH Health Systems pilot, being implemented by SughaVazhvu Healthcare in Thanjavur District of Tamil Nadu, calls for well-coordinated care pathways with the following six elements (as shown in the figure above):
- Mapping: For long term effective mapping of the health of a population, uniquely identifying the individual is instrumental. Pre-enrolment methodology that geo-maps and uniquely identifies individuals through bar-coded identity cards, ensure an organic growth of the personal health record of an individual.
- Screening: Comprehensive screening protocols, mapped with walk-in health centre based consultation protocols allow effective tracking of both chronic conditions and episodes of acute illness.
- Cohort Tracking: Managing populations and mapping their chronic high risk parameters is as essential as pure disease management at the village-level.
- Interventions: Defining the complete primary care value proposition is instrumental to ensure the success of our pilot. Within the Indian rural healthcare context, near complete primary-care value-proposition is essential (accompanied by aural, ophthalmic and basic oral hygiene capability) as minimal services are unavailable in the vicinity.
- Referral Services: As we evolve in our journey, effectively coupling our primary-care delivery platform with referral channel towards higher level of care – secondary and tertiary will allow us to demonstrate a functional managed-care platform for rural Indian populations.
- Fixed Annual Cost: An annual fixed premium will enable enrolled members to access healthcare services through our delivery model at all levels of care (including secondary and tertiary care).
Primary healthcare as provisioned directly through the network of SughaVazhvu Rural Micro Health Centres (RMHC) compares well with a Staff HMO Model. Whereas for referral towards secondary and tertiary care services it is more like a traditional hospital indemnity plan. If primary care services at a RMHC are extended to non-enrolees through a fee-for-service model then rather than a pure-HMO, SughaVazhvu compares better to a hybrid health maintenance organisation. Managed care evolved to deal with curative services and the classification is based on the clientele utilizing primarily curative care services. If SughaVazhvu RMHCs service only enrolees and refer all the other walk-ins to a Primary Health Centre (PHC), then SughaVazhvu classifies as a pure HMO. The population based enrolment and rapid risk assessment services offered by SughaVazhvu Healthcare are positive externalities to non-enrolees and will not distinguish SughaVazhvu from being a pure-managed to a hybrid health maintenance organisation.


Leave a Reply
Be the First to Comment!