By A.R. Selva Swetha, Research Analyst – ICTPH
A key element to the ICTPH Health System Design is protocolisation. All interactions right from patient management at the Rural Micro Health Clinic (RMHC)-level, to patient follow-ups, to household-level surveys and risk-profiling exercises have their basis in a framework of standard protocols. Central to the idea here is the creation of an Atul Gawande-style “Checklist” environment, ensuring process standardisation and minimising the scope for error. Providing a strong backbone to this Protocolised Patient Management is our Health Management Information Systems (HMIS), technological facilitation acts as a strong catalyst to foster a ‘Checklist’ culture of systemized patient management.
For every patient visit to the clinic, an end-to-end protocol for the workflow is laid out, and all information is captured on the HMIS replete with time-tags. The first point of interaction at the RHMC is the Health Extension Worker (HEW) who performs a one-time comprehensive screening (called the Population-based Individual level Screening Protocol or PISP) upon the patient’s first visit, and thereafter performs routine screenings and vital measures for the patient’s every visit. It is only after the session with the HEW that the doctor consults with the patient.
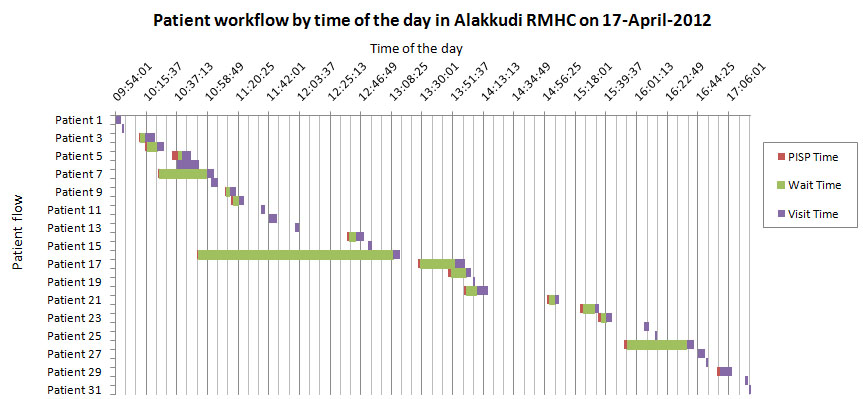
Here’s a look at the analysis the patient flow of Alakkudi RHMC. This is experimentally being run as a free-clinic with the intention of simulating a Government-run PHC setting, where the removal of that all-important financial barrier to seeking care may well change health behaviour. We intend here, to evaluate health outcomes and also stress-test the adherence to our process protocols in such an environment.
This analysis was done on the patient traffic on 17th April 2012, where we saw 31 patient visits. We wanted to look at whether full process adherence was happening, if patients were visiting in bunches at certain times of the day, whether we needed to cap the patient load at a certain level and allow the HEW the discretion to triage and prioritise the urgent patients.
Here is the chart showing patient flow by time of day: for each patient, the time spent is broken down into the time spent for PISP, the wait time between PISP and consultation, and the time spent during consultation.
Average time per PISP: 1:51 minutes
Average time per consultation: 04:32 minutes
Average wait time between PISP and consultation: 11:06 minutes (Having excluded the one outlier of 2 hours, 17 minutes)
Maximum consultation time: 15:16 minutes
Minimum consultation time: 01:30 minutes
If broken down by first time visit and non-first-time visit, (Assumption here is that if the PISP was done at that visit, it was a first time visit)
Average consultation time for first time visit: 05:12 minutes
Average consultation time for non-first-time visit: 03:50 minutes
Of course, the numbers in the chart don’t tell the whole story, for a lot of things go uncaptured right now in these HMIS time tags:
- HEW searching for the individual on the database / creating temporary ID (2 minutes per patient for 50% of patients)
- Explanation of the PISP report by the HEW (1.5 minutes, 50% of patients)
- Cervical Examination (12 minutes, 10-15% of patients a day)
- Time taken to draw the blood for CVD tests. (2 draws of blood including one with glucose load) (5 minutes, 10-15% of patients)
- After submission of the visit on the HMIS is when the doctor dispenses medication, instructs the patient on their usage, etc. (2 min)
- Printing of bill by HEW (0.5 min)
Factoring all this in, time spent on average per patient would be about 15 minutes.
Time available to HEW attend to patients is ~6.5 hours (Taking into account routine duties – patient follow-up calls, autoclaving, centrifuging)
Time available to doctor to interact with patients ~7.5 hours (taking into account his duties of supervising HEW follow-ups, ensuring adequate inventory, etc.)
Factoring in the dependencies in the critical path, let’s say the total time available is 7*1.5, i.e., 10.5 hours.
So, number patients that can be seen on average per day at 15 minutes per patient is theoretically around 42 patients.
However the real capacity that the clinic can comfortably handle on a daily basis without the clinicians being too overstretched may well be around 35 patients. Depending on patient footfalls, we may consider capping the patient load at around 30 and allowing for 5 emergencies. Now these HMIS entries are audited at the Thanjavur Headquarters at the back-end in near real-time. As a next step, we would be looking to add to the current audit parameters of clinical accuracy and process compliance, a third dimension of minimum time being spent per patient. This will not only allow us to get a better sense of the patient visit but also allow us to iterate and continuously improve on the processes set, in order to better optimise patient experience.


Leave a Reply
Be the First to Comment!